Injection-Site Pain
Which factors influence pain upon subcutaneous injection?
Biologics such as vaccines, insulin, monoclonal antibodies, etc., that are now widely developed need to be administered parenterally.
While the intravenous (IV) route has historically been the most widely used, the subcutaneous (SC) route is now accepted and presented as safe and effective, whether in the context of chronic disease or in palliative care.
The SC route of administration presents certain advantages over other parenteral routes, such as bioavailability, easiness compared to IV, and limited risk of infection. It also offers a broader choice of injection site, compared to the intramuscular (IM) route for instance.1 Ultimately, it can reduce treatment burden and improve patient’s quality of life by allowing self-administration.2
However, the SC route is also known and described to be associated with some discomfort and local pain which altogether can compromise patients’ adherence to treatment.
What are the factors influencing injection site pain and local inflammation?
What triggers pain during and after an injection?
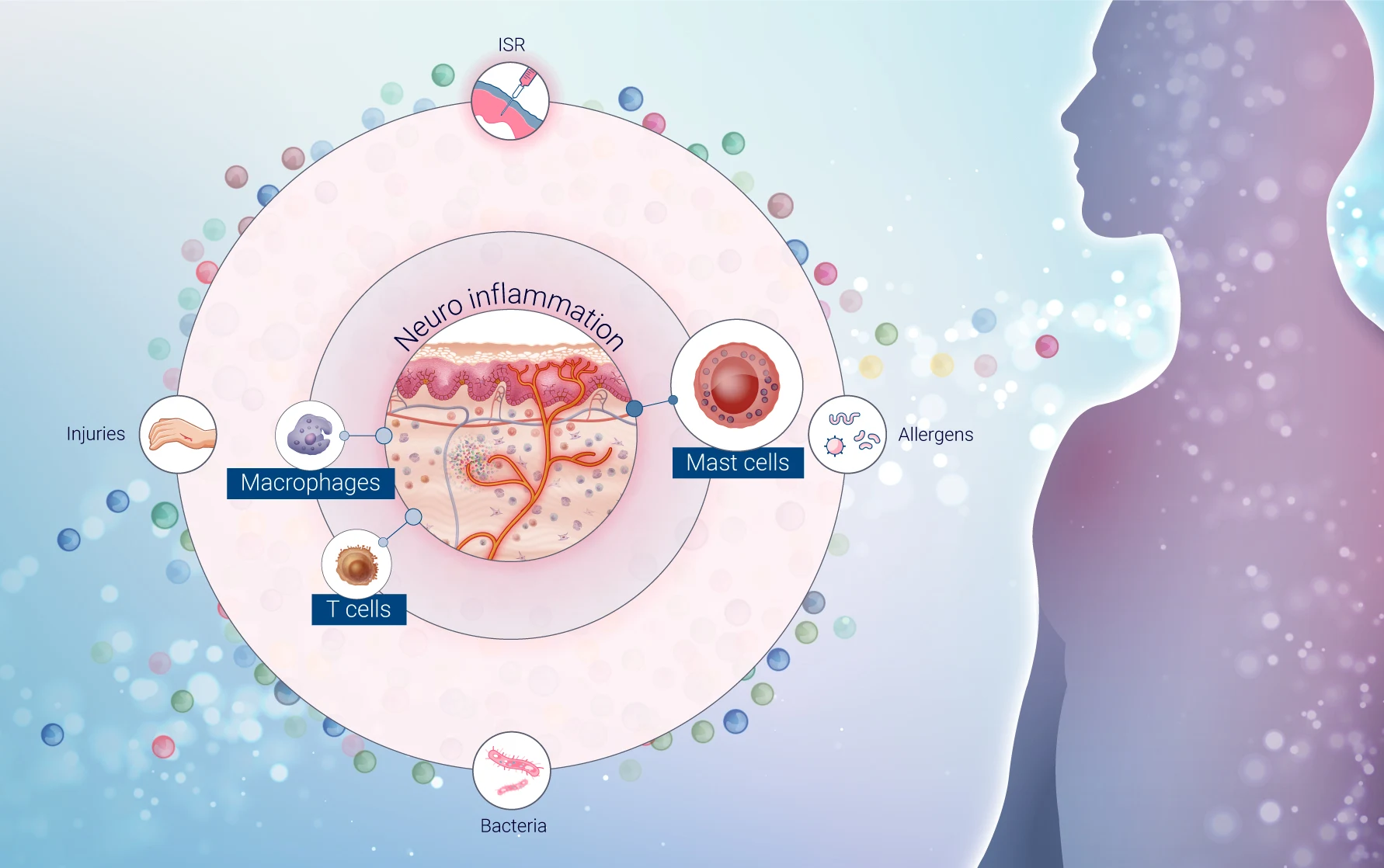
Different factors can influence the sensation of pain following injection. Pain itself is a complex mechanism. Pain after injection is a complex response influenced by four key factors contributing to neurogenic inflammation at the injection site:
- Device type and needle features
- Formulation factors
- Delivery factors
- Patients factors3
St Clair-Jones et al. have grouped these factors into three categories as follows:
- Product-related factors: These include the device, needle type, and formulation characteristics.
- Injection-related factors: These are similar to delivery factors.
- Patient-related factors: These remain unchanged from the original categorization.4
| Nature of factor | Detail |
|---|---|
| Product-related | • Device type (needle-free) • Needle type (sharpness, length, diameter…) • Osmolality • Viscosity • pH and buffers • Preservatives • Impurities |
| Injection-related | • Pinch technique • Penetration angle (also related to needle/device) • Injection speed (also related to device type) • Injected volume • Temperature • Location of injection |
| Patient-related | • Anxiety • Fatigue |
Now, let’s dive into these different factors and how they influence the discomfort felt after subcutaneous injections.
Device type & needle features
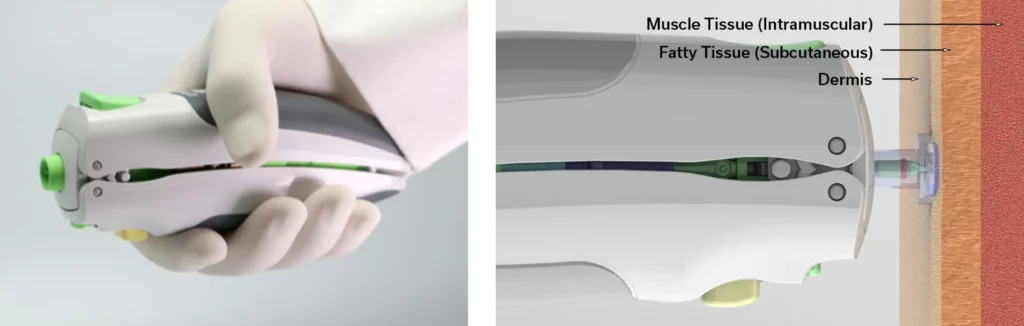
The choice of device type and the needle features can significantly influence pain during subcutaneous injections. Key factors include needle length, diameter, tip sharpness, bevel type, and lubricity. Shorter and smaller diameter needles generally cause less pain, bleeding, and bruising. Recommended lengths are 4–8 mm for adults and 4–6 mm for children. Advanced needle tips and silicone coatings reduce pain and insertion resistance but can cause protein aggregation of the drugs. New non-injectable subcutaneous systems are being developed, offering virtually painless, efficient drug delivery. Some of these devices are FDA-approved, such as the needle-free injectors Tropis® and Stratis®, respectively for intradermal and SC/IM administration, from PharmaJet.
Ultimately, a patient’s preference for a certain type of device may vary and should also be taken into account. Patients with needle anxiety might prefer pre-filled autoinjector pens, in which the needle cannot be seen.4
Formulation factors
Product-related factors differ between biologics as well as for an approved therapeutic and its biosimilar,4 especially when it comes to formulations.
Formulating injectable products to minimize pain involves several considerations. Ideally, these products should be isotonic, but hypertonic solutions (up to 600 mOsm/kg) are sometimes used to reduce injection volume, although higher osmolality can increase pain. Low viscosity solutions tend to be more painful, whereas higher viscosity (up to 15–20 cP) injections are better tolerated.3
Maintaining a near-physiological pH is crucial to reduce pain, irritation, and tissue damage; as extreme pH values can cause severe adverse effects. Buffers like citrate, phosphate, and acetate are used to adjust pH and optimize stability. Studies show that higher buffer concentrations can increase pain. For instance, 10 mM phosphate at pH 7 is less painful than higher concentrations or different pH levels. Citrate buffers, especially at higher concentrations (e.g., 23 mM), have been associated with increased pain, leading to a shift towards formulations with lower citrate content.3
A paper from Gely et al. published in 2020 measured the pain intensity after administration of two different formulations of adalimumab, one with citrate and the other without. The paper concluded that “Improved formulations for subcutaneous administration of drugs can positively impact patients’ convenience and adherence.”5
Preservatives in multi-dose preparations, such as phenol, benzyl alcohol, and m-cresol, can also influence pain levels. Phenol and benzyl alcohol generally cause similar pain levels, but m-cresol can result in more painful injections.
Furthermore, adding sodium bicarbonate to buffer local anesthetic solutions like lidocaine and bupivacaine can reduce injection pain by increasing pH, enhancing anesthetic effectiveness.
In summary, to minimize pain, injectable formulations should aim for isotonicity, appropriate viscosity, near-physiological pH, and careful selection and concentration of buffers and preservatives. Adjustments in these parameters can significantly influence the sensation of pain at the injection site.
Delivery factors
When performing SC injections, the recommended angle is 45° or 90° using the pinch technique4, depending on needle length and subcutaneous tissue. A 45° angle, with the needle bevel up, is advised for needles 8 mm or longer to reduce pain. Needle length must be adequate to reach the hypodermis without hitting muscle, as IM injections cause faster drug absorption, higher pain, and greater risks, like hypoglycemia with insulin.3
Studies evaluating the effect of injection speed on pain show inconsistencies and no significant differences in pain perception with varying speeds.4
The maximum volume generally accepted for an SC injection is around 1.5 ml, though up to 4 ml can be administered if necessary. While larger volumes are often associated with increased pain, data is conflicting; volumes of 1-1.5 ml may cause more pain than 0.5 ml or less, but up to 3 ml can be well tolerated in the abdomen. Thigh injections are more painful than abdominal, but injection volumes up to 0.8 ml typically do not increase pain in either site.3
Repeated use of the exact same site for injection has shown to increase irritation and injection site pain. It is recommended to rotate injection sites.3
The temperature of the solution can also have an impact on pain. Biologics are usually stored at 2-8˚C but should be normalized to room temperature prior to being administered.4
Patient factors
The mechanism behind pain and neurogenic inflammation is real and complex but the experience of injection site pain (ISP) during SC injections can be felt differently by patients. While many patients report ISP, its intensity often decreases with repeated administrations, leading to increased tolerance. Factors such as female gender, low body weight, fibromyalgia, depression, and severe rheumatoid arthritis increase the likelihood of greater ISP.
Injection anxiety affects up to 20% of individuals, often due to concerns over self-injection accuracy or needle phobia. Interestingly, professional administration of biologics is associated with more ISP than self-administration. Psychosocial factors, such as pain catastrophizing and the nocebo effect3, can heighten pain perception. These cognitive and emotional responses significantly impact patient-reported outcomes, regardless of age, gender, or disease duration.
Moreover, patients may struggle to articulate ISP, leading to underreported discomfort. When prompted, concerns about the injection experience often surpass safety issues as reasons for discontinuing SC treatments.
How can an ex vivo human skin model, lacking sensory nerves, provide valuable insights into the neurogenic inflammation and pain mechanisms triggered by injections?
Pain is a complex mechanism, and injection site pain depends on numerous factors. While these factors are known, there are no universal rules to rely on, as formulations and devices must be tailored to specific active compounds.
Testing products ahead of time in a reliable system is crucial to ensure smooth clinical outcomes, patient comfort, and adherence. Understanding the mechanisms of pain allows us to better assess and compare formulations to select the most promising candidates.
Genoskin’s ImmunoSafe: ISR platform®, powered by HypoSkin®, is one of the most accurate testing alternatives to human trials. It provides more predictive outcomes for human responses compared to traditional animal testing methods and accelerates development timelines.
By comprehending the mechanism of neurogenic inflammation and utilizing multiplex cytokine analysis and transcriptomics, we can identify the involved pathways and anticipate injection-site pain. The ImmunoSafe: ISR Platform® enables the prediction of injection site pain before clinical trials, facilitating the selection of the optimal drug candidate or the enhancement of formulations.
Sources
1Dubin AE, Patapoutian A. Nociceptors: the sensors of the pain pathway. J Clin Invest. 2010 Nov;120(11):3760-72. doi: 10.1172/JCI42843. Epub 2010 Nov 1. PMID: 21041958; PMCID: PMC2964977.
2Chap 13.1. Oregon State University – Anatomy and Physiology. https://open.oregonstate.education/aandp/chapter/13-1-sensory-receptors/
3Woller SA, Eddinger KA, Corr M, Yaksh TL. An overview of pathways encoding nociception. Clin Exp Rheumatol. 2017 Sep-Oct;35 Suppl 107(5):40-46. Epub 2017 Sep 29. PMID: 28967373; PMCID: PMC6636838.
4Chiu IM, von Hehn CA, Woolf CJ. Neurogenic inflammation and the peripheral nervous system in host defense and immunopathology. Nat Neurosci. 2012 Jul 26;15(8):1063-7. doi: 10.1038/nn.3144. PMID: 22837035; PMCID: PMC3520068.
5Scott A.Armstrong, Michael J. Herr. Physiology, Nociception. Statpearls, NIH (https://www.ncbi.nlm.nih.gov/books/NBK551562/)
6Pinho-Ribeiro et al. Nociceptor Sensory Neuron–Immune Interactions in Pain and Inflammation, Trends in Immunology, January 20217, Vol.38, N˙1. http://dx.doi.org/10.1016/j.it.2016.10.001
7Marek-Jozefowicz, L.; Nedoszytko, B.; Grochocka, M.; Żmijewski, M.A.; Czajkowski, R.; Cubała, W.J.; Slominski, A.T. Molecular Mechanisms of Neurogenic Inflammation of the Skin. Int. J. Mol. Sci. 2023, 24, 5001. https://doi.org/10.3390/ijms24055001
8Green, D. P., Limjunyawong, N., Gour, N., Pundir, P., & Dong, X. (2019). A Mast-Cell-Specific Receptor Mediates Neurogenic Inflammation and Pain. Neuron, 101(3), 412–420.e3. https://doi.org/10.1016/j.neuron.2019.01.012
Comments are closed.

